Introduction:
Welcome to our comprehensive guide on corneal ulcers. In this article, we aim to provide you with detailed information about corneal ulcers, including their causes, symptoms, and available treatment options. We, as a leading source of expert knowledge in the field, are dedicated to delivering accurate and helpful content to help you better understand and manage corneal ulcers.
Understanding Corneal Ulcers:
What is a Corneal Ulcer?
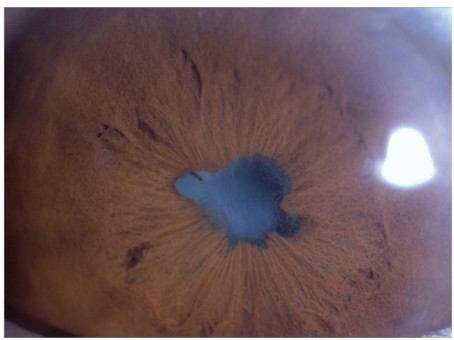
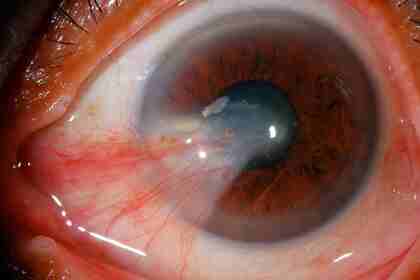
A corneal ulcer also known as microbial keratitis, is an infection of the cornea, which is the clear window in the front of our eyes.

Common Causes of Corneal Ulcers:
- Bacterial Infections: Bacteria, such as Staphylococcus aureus or Pseudomonas aeruginosa, can invade the cornea through a scratch or other forms of trauma.
- Viral Infections: Viruses, particularly the herpes simplex virus (HSV), can cause corneal ulcers, often leading to recurring episodes.
- Fungal Infections: Fungi, like Fusarium or Aspergillus, can infect the cornea, particularly in individuals who wear contact lenses.
- Trauma: Any injury to the cornea, such as a scratch from a foreign object or accidental eye poking, can create an entry point for infections and result in corneal ulcers.
- Dry Eye Syndrome: Insufficient lubrication of the eyes can lead to corneal damage and ulcers.
- Contact Lens Misuse: Wearing contact lenses for extended periods or poor hygiene practices can increase the risk of corneal ulcers.
- Underlying Eye Conditions: Certain conditions, such as blepharitis (eyelid inflammation) or keratitis (corneal inflammation), can predispose individuals to corneal ulcers.
Factors Contributing to Corneal Ulcers:
Corneal ulcers primarily develop as a result of corneal injury or trauma, such as a cut to the cornea.
When bacteria, fungi, or viruses infiltrate a specific area of the cornea that is already damaged, they can cause an infection and lead to the subsequent formation of an ulcer. In addition to corneal injury, several other risk factors contribute to the development of corneal ulcers. These factors include:
- Unhealthy Cornea: Patients with pre-existing conditions such as uncontrolled diabetes, malnutrition, malignancy, or individuals taking immunosuppressive medications are more prone to corneal ulcers. A compromised cornea is more vulnerable to infections and less capable of healing efficiently.
- Prolonged Contact Lens Wear: Individuals who wear contact lenses for extended periods of time are at an increased risk of corneal ulcers. Insufficient lens hygiene, inadequate lens disinfection, and improper lens replacement can create an environment conducive to bacterial growth and increase the likelihood of corneal ulcers.
- Sleeping with Contact Lenses: Sleeping while wearing contact lenses significantly raises the risk of corneal ulcers. During sleep, contact lenses impede oxygen flow to the cornea, promoting bacterial growth and increasing the chances of developing ulcers. Unless specifically instructed by an eye care professional, it is crucial to remove contact lenses before sleeping.
- Use of Steroid Drops: Prolonged use of steroid eye drops without appropriate medical supervision can weaken the cornea’s natural defense mechanisms and thin its structure. This can make the cornea more susceptible to infections, including corneal ulcers. It is essential to follow the prescribed dosage and duration when using any medication, including steroid eye drops.
- Eyelid Abnormalities: Abnormalities of the eyelids, such as lashes turning inwards (entropion), can cause chronic irritation to the cornea. The constant friction and abrasion from the inverted lashes can lead to corneal ulcers over time. Addressing eyelid abnormalities through corrective measures, including surgical intervention if necessary, is important to reduce the risk of corneal ulcers.
Organisms Responsible for Corneal Ulcers:
A number of microorganisms such as bacteria, viruses, fungi, or even parasites can cause corneal ulcers. In colder climates, bacteria commonly cause them, while fungal infections are more frequently observed in tropical climates but can also occur in certain at-risk individuals.
Viral infections are typically caused by the Herpes virus family, such as the Herpes Simplex Virus or Varicella Zoster Virus, which is responsible for chickenpox or shingles.
Symptoms of Corneal Ulcers:
Some common symptoms include:
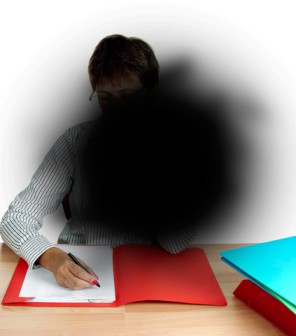
• Blurring of vision
• Eye pain
• Sensitivity to light
• Redness
• White patch on cornea
Call Us Now
Diagnosing Corneal Infections:
The Ophthalmologist may take samples from the cornea (a scrape) or swab from the surface of the eye to send to a laboratory. The contact lens solution and contact lenses can also be sent to the laboratory for testing. This can help in confirming the diagnosis, identifying which microorganism has caused your infection and guiding the best treatment to use.

Treatment for Corneal Ulcers:
The treatment of the ulcer depends on its severity:
1. Superficial Infections: Infections limited to the surface of the eye are typically treated with intensive antiseptic eye drops or ointments. These medications contain antibiotics or antiseptic agents to combat the infection. The ophthalmologist may monitor your response to treatment and adjust the medication regimen accordingly. If necessary, the antibiotics may be changed or increased based on laboratory findings or your individual response.
2. Deeper Infections (Involving the Corneal Stroma): If the deeper layer of the cornea, known as the stroma, is affected, the treatment approach may require additional measures. Inflammation often accompanies such infections, and in these cases, steroid eye drops may be prescribed to reduce the inflammation. It is important to note that the use of steroid eye drops should be strictly supervised by an eye doctor. While they effectively reduce inflammation, improper use can worsen the infection. Regular follow-up visits with the ophthalmologist are essential to monitor progress and ensure the appropriate use of steroid medications.
The treatment of corneal ulcers is a delicate balance between eradicating the infection and minimizing potential complications. Along with the prescribed medications, it is vital to follow proper eye hygiene practices and adhere to the recommended treatment regimen. Be sure to communicate any changes in symptoms or concerns to your ophthalmologist promptly.
Complications of Corneal Ulcers:
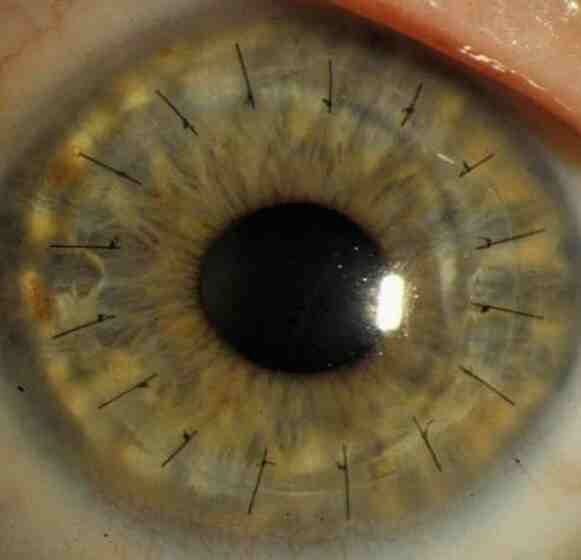
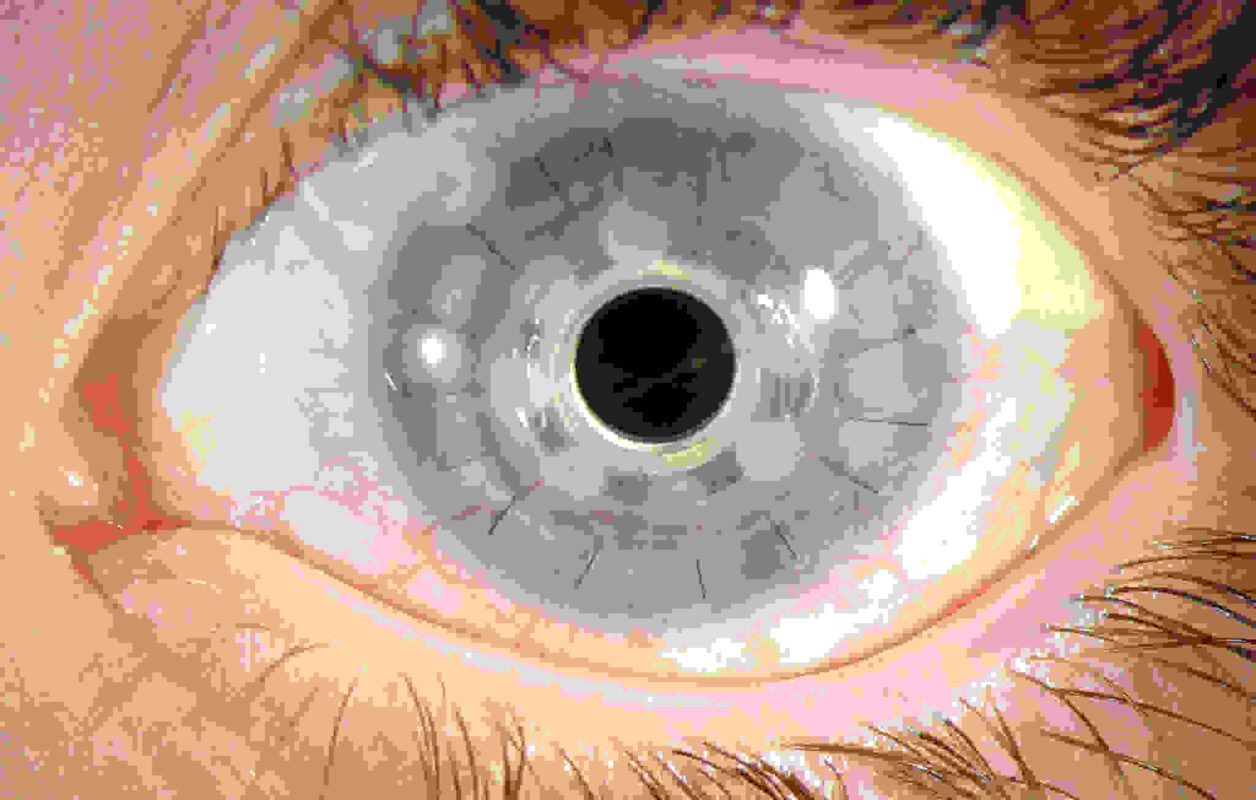
- Corneal Melting: In certain cases, corneal ulcers can lead to severe inflammation of the cornea, causing it to melt. Corneal melting involves the progressive breakdown and liquefaction of corneal tissue, leading to a weakened cornea and the potential for corneal perforation. Corneal melting is a serious complication that may necessitate surgical intervention in an attempt to seal the perforation and stabilize the cornea.
- Vision Limitations: Corneal scarring and the growth of blood vessels into the cornea (corneal neovascularization) can severely limit vision. Corneal scarring results in a permanent alteration of the cornea’s transparent structure, leading to blurred or distorted vision. Moreover, blood vessel growth into the cornea can disrupt its clarity and interfere with visual acuity. In cases where vision is significantly compromised, surgery may be considered.
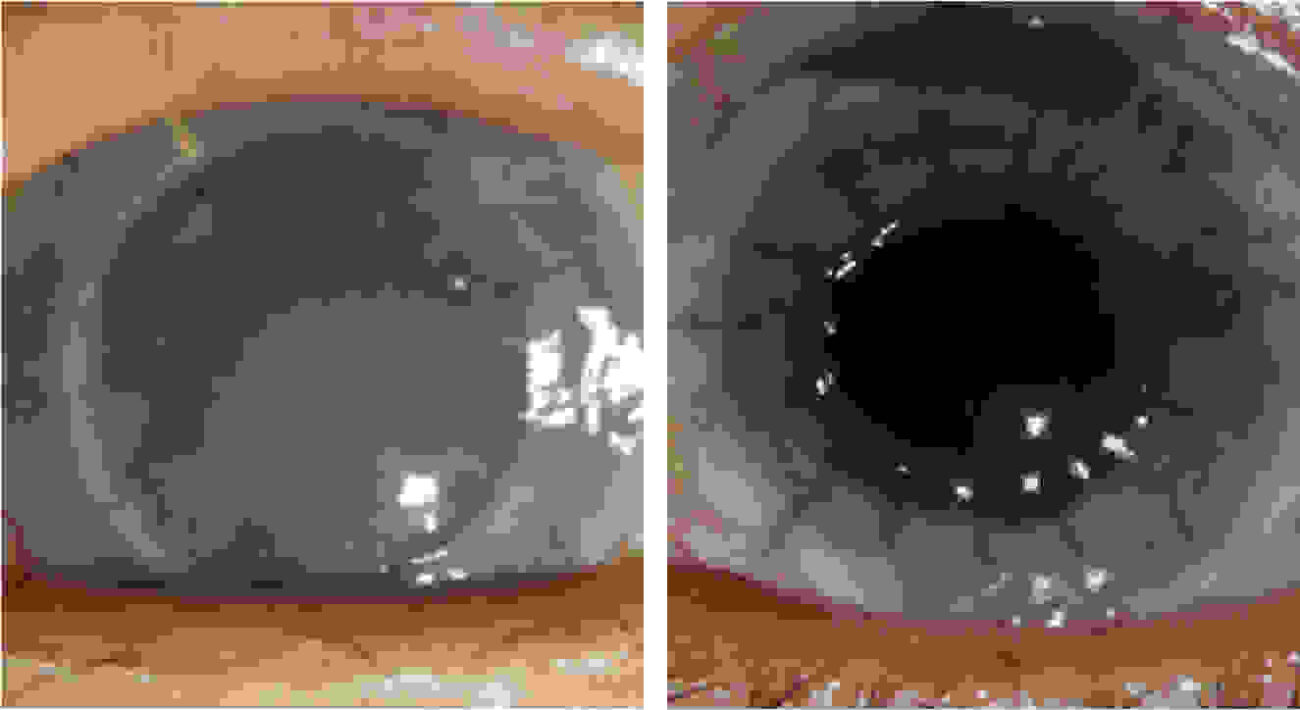
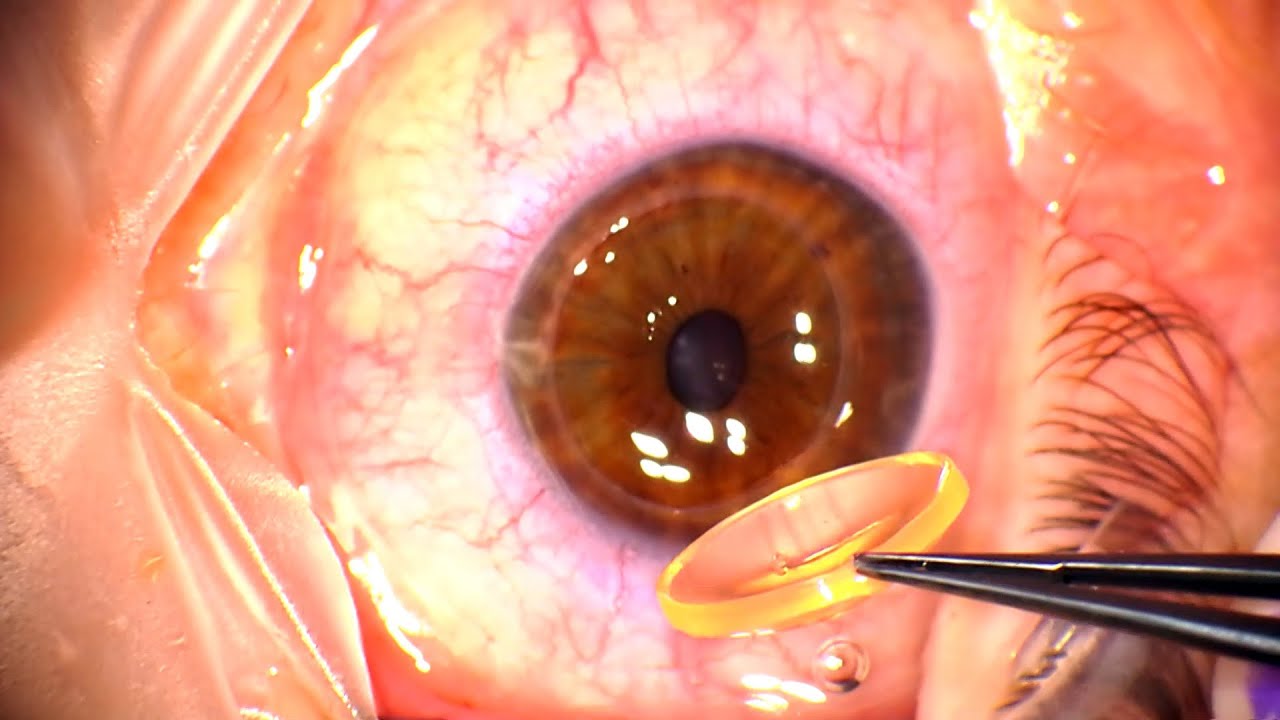
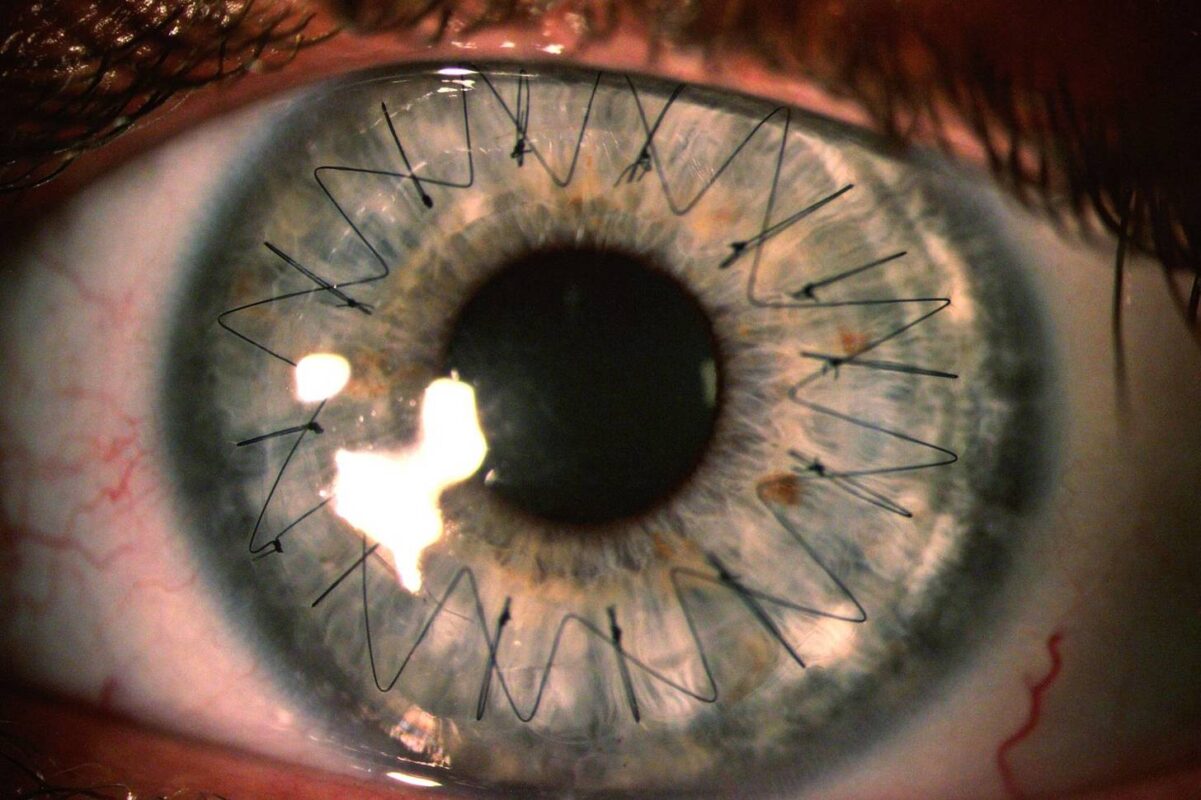
In situations where vision limitations persist despite conservative treatments, surgical options such as corneal transplant or keratoplasty may be recommended. During a corneal transplant, the damaged cornea is replaced with a healthy cornea obtained from a donor. This procedure aims to restore vision by removing the scarred or compromised cornea and replacing it with a clear cornea. The specific type of corneal transplant (e.g., full-thickness or partial-thickness) will depend on the individual’s condition and the extent of corneal damage.
It is important to note that the decision to pursue surgery is made on a case-by-case basis and requires a thorough evaluation by an ophthalmologist. Surgical intervention is typically considered when non-surgical treatments have been ineffective or when the severity of the complications warrants a more aggressive approach.
If you experience worsening symptoms, such as increased pain, sudden changes in vision, or signs of corneal perforation, it is crucial to seek immediate medical attention.
Book Your Appointment Now
Key Considerations for Corneal Ulcer Management:
Do not wear contact lenses during the acute infection Wearing sunglasses can make you feel more comfortable during an infection.
Steroid eye drops should only be used under close supervision of an ophthalmologist.
Author Details:
Dr. Sinchana Adyanthaya is a dedicated ophthalmologist with a wide range of experience. She has excelled in routine OPD work, managed high-volume OPDs, and performed various eye procedures. Her fellowship in Cornea and Refractive Surgery has enhanced her skills in advanced corneal investigations and surgeries. Dr. Adyanthaya has published research articles, presented at conferences, and actively participated in academic activities. With her proficiency in multiple languages, she ensures effective communication with patients. Overall, she is a skilled and compassionate ophthalmologist committed to providing excellent care.

Consult Now
Conclusion:
In conclusion, corneal ulcers demand immediate attention. Swift action and timely treatment are vital to safeguard vision. Recognize symptoms, avoid contact lenses during infection, and wear sunglasses for comfort. Follow medical advice closely, prioritize eye health, and seek professional care promptly. By taking these steps, you can protect your eyes and ensure a brighter future for your vision.