A corneal ulcer is an open sore on your cornea. Infection is the leading cause. Symptoms include a red, watery and bloodshot eye; severe eye pain and pus or other eye discharge. A corneal ulcer can lead to vision loss and blindness. It’s considered a medical emergency. Contact your eye care provider right away if you have symptoms of a corneal ulcer.
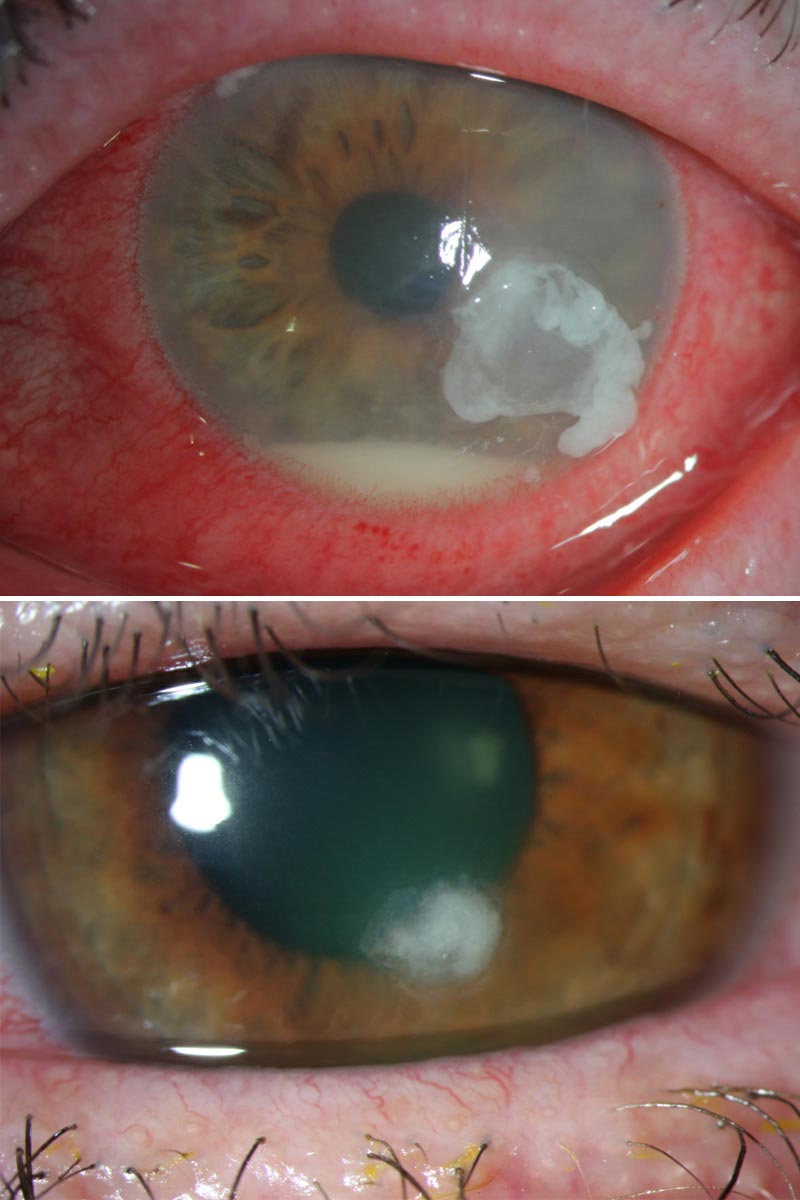
A corneal ulcer is an open sore on your cornea. Your cornea is the dome-shaped clear tissue layer that covers the front of your eye. Infection is the most common cause of a corneal ulcer.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
You’re at risk of a corneal ulcer if you:
In the U.S., between 30,000 and 75,000 corneal ulcers occur each year. About 12% of all corneal transplants are done due to a corneal ulcer.
A corneal ulcer can cause permanent damage, even blindness if it’s not treated. If you think you have a corneal ulcer or have any eye problems that bother you, contact your eye care provider right away.
Symptoms of a corneal ulcer include:
A corneal ulcer usually develops in one eye only.
Because a corneal ulcer can cause permanent vision loss, rupture your cornea and destroy the tissue in your eye socket, it’s a medical emergency. If you have symptoms of a corneal ulcer, seek immediate care. Corneal ulcers can cause blindness if not promptly treated.
Causes of corneal ulcers include:
Your eye care provider will:
Corneal ulcers are treated with anti-infective medications or surgery if medications aren’t an option.
Medication choice is based on what’s causing the infection. Eye drops containing antibiotics (for bacterial infections), antifungals (for fungal infections) and antivirals (for viral infections) are the usual treatments. Your eye care provider may sometimes choose oral medication (taken by mouth) or an injection, given near your eye.
Your eye care provider may also prescribe oral medication to reduce pain. Steroid eye drops are sometimes given to reduce eye inflammation and swelling. Because steroid drops may worsen an infection, you should follow your provider’s recommendations about their use. Your eye care provider will discuss this and all available treatment options.
You may need to take anti-infective medications frequently (every 1 to 2 hours) for several days. Your eye care provider will discuss how often to take your medications during your office visit.
Most corneal ulcers heal in two or three weeks.
Untreated corneal ulcers can lead to:
After the infection is gone from your cornea, scars that limit vision are common. A laser treatment called phototherapeutic keratectomy (PTK) can improve some scars. If a scar isn’t too deep, your provider may be able to use the laser to burn the scar tissue away and improve vision.
You may need a corneal transplant if:
In either case, you’ll need a new cornea to restore your vision. The tissue for a corneal transplant comes from a person who has recently died. The tissue is tested to make sure it’s healthy before the old corneal tissue is removed and the new tissue is stitched in place in your eye.
Complications include:
The best way to prevent a corneal ulcer is to see your eye care provider right away if you have an eye injury or think you have symptoms of a corneal ulcer.
Contact lens use is the highest risk factor for a corneal ulcer. With this in mind, some helpful tips for contact lens wearers include:
A corneal ulcer is a serious eye condition that can cause vision loss. Your outcome depends on the cause and location of the corneal ulcer. The earlier you see your eye care provider, confirm the diagnosis and start treatment, the better your outcome.
Contact your eye care provider right if you:
Wearing contacts for long period blocks oxygen from reaching your eyes. Also, bacteria on the lens — transferred from your finger when inserting or from non-sterile cleaning solutions — can get trapped under your lens. These factors raise the risk of infection, which can lead to a corneal ulcer.
A contact lens wearer is about 10 times more likely to get a corneal ulcer than someone who doesn’t wear contacts. Someone who sleeps in contact lenses is about 100 times more likely to get an ulcer than someone who doesn’t wear contacts.
A corneal abrasion is a scrape or scratch on your cornea. These corneal injuries usually heal on their own
A corneal ulcer is an open sore on your cornea. Infections, dry eye and other conditions cause a corneal ulcer.
These eye conditions are closely related.
A corneal ulcer is an open wound — a loss of corneal tissue — that’s often the result of an eye infection.
Keratitis is a more general term for a group of disease processes that cause inflammation of your cornea. Eye infection, injury and wearing contact lenses too long — some of the same causes of corneal ulcer — also cause eye inflammation. Keratitis can lead to a corneal ulcer.
Both conditions can lead to vision loss.
A note from Cleveland Clinic
Corneal ulcers are a vision-threatening eye emergency. Even a minor eye injury can lead to a corneal ulcer. If you think you have symptoms of a corneal ulcer, contact your eye care provider right away. They will examine your eye, make the diagnosis and start treatment. If you wear contact lenses, make sure you know how to properly insert, clean and store them. Your eye care team can teach you proper techniques and answer all your other questions.
Last reviewed by a Cleveland Clinic medical professional on 03/08/2022.
Learn more about our editorial process.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy